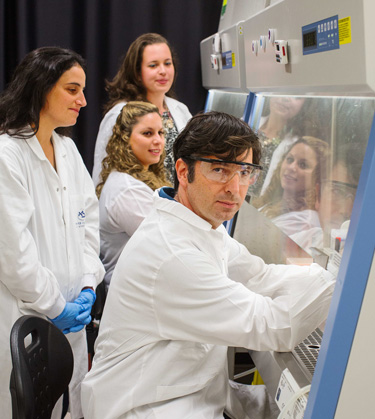
Dr. Ayal Hendel and team
Photo credit: Avishag Shar-Yashuv
For children suffering from sickle-cell anemia, cancer and immune diseases such as the “bubble boy” syndrome, the prognosis is bleak: pain, severe discomfort, difficulty in pursuing a normal lifestyle, and an uncertain future. But novel research underway in Dr. Ayal Hendel’s Genome Editing & Gene Therapy Laboratory at BIU’s Mina and Everard Goodman Faculty of Life Sciences may now offer promise and a new lease on life for countless youths.
Dr. Hendel is working to develop the innovative CRISPR technology — which employs a miniscule precision tool to help repair broken genes — thus leading the way to better treatment options for children suffering from genetic disorders. Recently, the gifted young Israeli scientist received a prestigious grant from the European Research Council (ERC) for his lab’s pioneering studies.*
“We’re developing technology that can actually correct broken genes,” explains Hendel, who joined Bar-Ilan University in 2016 following postdoctoral research at Stanford University School of Medicine (USA). “We use what I call cut-and-paste technology to replace broken genes with corrected genes.”
Working with the CRISPR (Clustered Regularly Interspaced Short Palindromic Repeats — named by Science as “2015 Breakthrough of the Year”) is pretty much like “working with scissors,” he notes. “All the DNA in our bodies is built from four different bases — A, T, G, and C. If there is one mistake, one typo in the code, it can lead to disorders, like ‘bubble boy’ or cancer. We use the CRISPR technology to cut out the broken gene and replace it with a synthetic normal gene.
“We can take blood — hematopoietic stem cells — from different sources, including cord blood (which some parents collect and freeze) and bone marrow. What happens when a kid has some genetic diseases? We can do what we call allogenic bone marrow transplant — we take the stem cells from somebody else — but many times we can’t find the right donor. The tissues aren’t the right match. In the technology we are developing, every patient can be his own donor.”
In the CRISPR technology, “the RNA functions like a GPS, headed for the target; the protein is the goon behind it, cutting out and demolishing the broken gene. And then the new, custom-made repair cell can be injected back into the patient. There is very sophisticated machinery inside ourselves that knows how to repair a break by using a piece of normal DNA,” says Dr. Hendel. He notes that the CRISPR system in nature is actually a bacterial defense mechanism.
“In order to protect itself against viruses — because when a virus attacks bacteria it injects it with its DNA — the bacteria can copy a small piece of the virus’s DNA and keep it in its memory. So the next time the same kind of virus attacks, the bacteria will have an image of the sequence of the DNA virus. It will know what to attack.”
For gene therapy applications, “different people have different mutations, so first you have to identify what went wrong, and you have to really get the right piece of DNA and the right correction. Once you are able to do that, you want to ensure that it is done in a very specific and safe way.” Brand-new changes can have unintended consequences; no one wants to attempt to heal someone and to start the butterfly effect that leads to a jumble of disasters and eventual collapse. Caution is necessary.
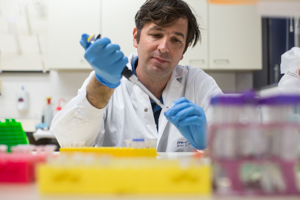
Photo credit: Avishag Shar-Yashuv
“This amazing genome editing technology — I call it iPhone 1.0 — was developed for the first time in 2003,” he said. “But then it was expensive, slow, and very difficult to work with. Then came iPhone 2.0 — but it was the third generation, iPhone 3.0, namely the CRISPR that really changed the field, because suddenly scientists had a tool that was cheap, easy to make and design, and really meant that many scientists could start working in parallel ways.”
Dr. Hendel focuses on Severe Combined Immunodeficiency or SCID (“bubble boy” syndrome) “because it is the result of just one typo in the DNA. It’s just one mutation that means that these kids can’t develop functional immune systems.
“So I chose this disease because there is a higher chance of success. If we cure only one to ten percent of the stem cells and put them back into the body, that will be enough to cure the disease. The body will be able to generate enough immune cells. It would be more challenging with other diseases; we would have to correct from 80 to 100 percent of the cells.”
He expects his own process to take about four or five years; then, he hopes, he will be able to start thinking about a clinical trial, maybe in collaboration with a large center in the United States or in Israel. “Now,” says BIU’s Dr. Ayal Hendel, “our mission is to build this DNA editor, so whenever there is a devastating mistake leading to childhood disorders, we can take the CRISPR and fix the origin of the problem.”
* Dr. Ayal Hendel is one of four BIU faculty members to have been awarded this highly competitive ERC grant in a single year.




